Section V: Summary —Today’s Shortcomings and Tomorrow’s Promise for Behavioral Health Care
A Framework for the Future
The SASH Stakeholder Executive Committee was asked to deliberate not only upon a new infrastructure for SASH, but also to reimagine an improved mental health system in South Texas. As we soon learned from stakeholders, it is clear that SASH, despite its vital role, impacts only a fraction of people with serious mental illness in our region. While about 280 people are hospitalized at SASH at any given time, over 76,000 people received services in the last fiscal year from one of the LMHA’s in SASH’s vast catchment area. This number does not include many others who seek services through private practices, private non-profit agencies or arrive at an emergency department of a local hospital in crisis.
It became clear in our deliberations that Texas today operates a “crisis-driven” public mental health system. Thousands of people remain outside the mental health system, often seeking access to it only when they are acutely ill due to psychosis, intoxication or suicidal thoughts. As Figure 13 depicts, we have become more skilled in reacting to these crises, through increased police training, coordinating law enforcement efforts, as well as short-term hospitalizations. Only a small minority of these patients are served by SASH. Many are discharged soon after stabilization, but the number who consistently avail themselves of the long-term treatment they require is far too few. This creates a cycle of “Crisis-Hospital-Discharge-Crisis” due to the factors illustrated by the red arrows.
What we have laid out in Figure 14 is an array of community supports that will lead to recovery for those with serious mental illness. In this model, we seek to prevent crises before they arise through a multifaceted approach of early intervention. Prevention now becomes a key feature.
 Once individuals have developed a serious mental illness, we must have a broader array of interventions. In rural areas, we need intensive services closer to home. When crises do arise, emergency departments should not have to play the anchoring role, but LMHA Crisis Centers and short-term hospitalizations can have a greater impact. Equally important, however, is the kind of after-care we provide to those leaving the hospital. These services, illustrated by the green arrows, seek to reduce relapse and rehospitalization, and enable patients to attain long-term recovery.
Once individuals have developed a serious mental illness, we must have a broader array of interventions. In rural areas, we need intensive services closer to home. When crises do arise, emergency departments should not have to play the anchoring role, but LMHA Crisis Centers and short-term hospitalizations can have a greater impact. Equally important, however, is the kind of after-care we provide to those leaving the hospital. These services, illustrated by the green arrows, seek to reduce relapse and rehospitalization, and enable patients to attain long-term recovery.
Ima Hogg, the daughter of James Stephen “Big Jim” Hogg who was Governor of Texas from 1891-1895, established the Hogg Foundation for Mental Health in memory of her brother Will in 1930. She developed her interest in mental health from visiting patients at the Austin State Hospital during her father’s term as Governor. She also suffered from depression herself, for which she was hospitalized. In a 1970 interview, she recalled, “I was also very much interested in mentally ill people in hospitals… My father was very interested, also… And often I went through with him and I’d hear him say to the superintendent or the doctor, ‘What can be done for these people? What are you doing?’”
Let us ask ourselves this question as we move forward to a new mental health system for South Texas.
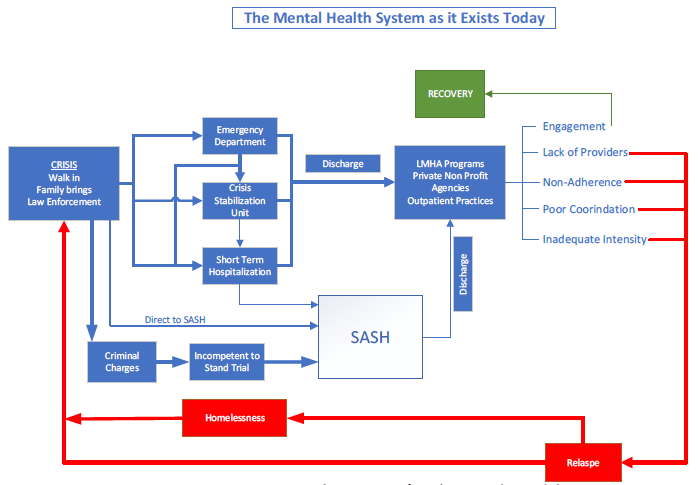 Figure 13: A Reactive, Crisis-Oriented System of Behavioral Health Care
Figure 13: A Reactive, Crisis-Oriented System of Behavioral Health Care
The mental health system of today is focused on response to crisis. The region’s Emergency Departments are often the first responders to mental health issues. The thickness of the arrows in the diagram indicated the most utilized pathways in the current system. Many patients, after stabilization of an acute crisis, fail to engage the treatments that lead to recovery. Instead, a variety of barriers lead to relapse, homelessness and new crises. In addition to replacing SASH, the mental health system must be re-imagined.
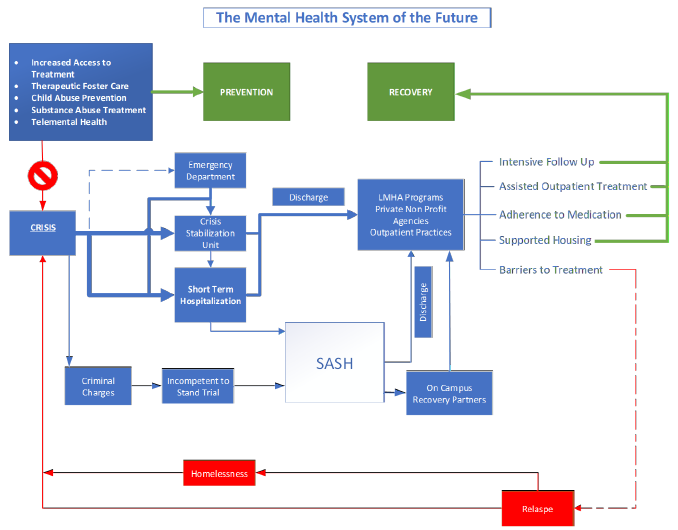 Figure 14: A Proactive, Patient-Centered and Prevention-Oriented System of Behavioral Health Care
Figure 14: A Proactive, Patient-Centered and Prevention-Oriented System of Behavioral Health Care
Through early intervention and expansion of services, mental health crises can be avoided, either by preventing the development of mental illness or by intervening well before crisis. Once a patient is hospitalized, a discharge process should involve a wide range of interventions beyond traditional outpatient services. This will enhance recovery.