Tetralogy of Fallot
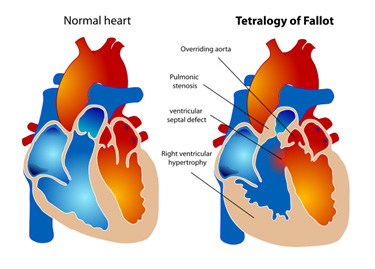 Tetralogy of Fallot refers to the constellation of VSD, right ventricular outflow tract (RVOT) obstruction (ie: pulmonary stenosis), right ventricular hypertrophy (RVH), and an overriding aorta.
Tetralogy of Fallot refers to the constellation of VSD, right ventricular outflow tract (RVOT) obstruction (ie: pulmonary stenosis), right ventricular hypertrophy (RVH), and an overriding aorta.
The VSD is usually large and unrestrictive, and the direction and severity of shunting depend upon the degree of RVOT obstruction.
The higher the obstruction to blood flow exiting the RV to the PA, the more blood which will be forced across the VSD. This in turn determines the degree of cyanosis and the age of presentation.
Patients with mild RVOT obstruction may have normal oxygen saturations and predominantly left-to-right shunting through the VSD (acyanotic or “pink” tetralogy), while those with severe RVOT obstruction will have significant right-to-left shunting and present early in infancy with cyanosis. Cyanosis is usually mild at birth and gradually progresses with age as RVH and RVOT obstruction worsen.
Cyanotic “tet spells” are periods of profound hypoxemia that may be induced by dehydration, respiratory infection, or peripheral vasodilation from medications, resulting in a marked decrease in pulmonary blood flow and increase in the right-to-left shunt across the VSD.
Patients usually have a midsystolic ejection murmur best heard at the left 3rd intercostal space, and is related to the VSD. CXR may show a “boot-shaped” heart, and a right-sided aortic arch is present 25% of the time. Echocardiogram will show the typical malalignment VSD with aortic override and RVOT obstruction.
Coronary abnormalities may be present and can often be seen on echocardiogram. Cardiac catheterization is usually not performed prior to surgery unless specific questions arise. Lab studies to detect a deletion on chromosome 22 are also performed, as conotruncal anomalies may arise as part of a syndrome, the most severe form being DiGeorge syndrome.
 Most children have adequate oxygen saturations at birth and can be allowed to grow and await elective repair. Prior to repair, children should be kept well hydrated and free from viral infections to avoid spells. If saturations fall below 75-80%, or if patients are experiencing cyanotic spells, surgical repair should be performed. Otherwise, elective repair is recommended by 6 months of age.
Most children have adequate oxygen saturations at birth and can be allowed to grow and await elective repair. Prior to repair, children should be kept well hydrated and free from viral infections to avoid spells. If saturations fall below 75-80%, or if patients are experiencing cyanotic spells, surgical repair should be performed. Otherwise, elective repair is recommended by 6 months of age.
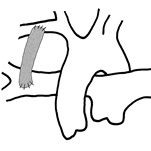
Palliative surgery may be performed by using a number of different shunts, all of which have the common goal of establishing blood flow to the pulmonary arteries (see most common, the modified Blalock Taussig shunt, below).
Modified Blalock Taussig Shunt used for palliation:
The subclavian artery gives blood to pulmonary artery via Gor-Tex graft.
Complete repair addresses the features of TOF and includes patch repair of VSD, ligation of any existing systemic to pulmonary shunts (congenitally and/or surgically created), and alleviation of the RVOT obstruction.