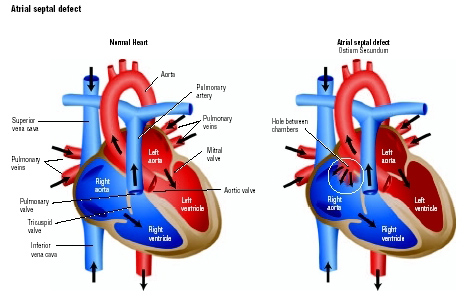
Atrial Septal Defect (ASD)
ASDs constitute 8-13% of all congenital heart defects. There are three main types of ASDs. The most common is the ostium secundum, which arises within the boundaries of the fossa ovalis. A primum ASD results from persistence of the ostium primum and is associated with atrioventricular canal defects. A sinus venosus defect usually occurs high on the septum close to the orifice of the superior vena cava (SVC) and is associated with partial anomalous pulmonary venous connection (PAPVR). A rare type of ASD is the coronary sinus defect, which results from unroofing of the coronary sinus as it courses along the left atrial floor.
Patients with an isolated ASD are usually without symptoms. An echocardiogram is used to define the defect. If performed, cardiac catheterization would show a “step-up” in oxygen saturation between the SVC and right atrium (RA) due to mixing.
 In 1952, Drs Lillihei and Lewis performed the first ASD closure, by using cooling blankets to lower the child’s core body temperature to temporarily stop the heart. The surgery had to be completed in under ten minutes.
In 1952, Drs Lillihei and Lewis performed the first ASD closure, by using cooling blankets to lower the child’s core body temperature to temporarily stop the heart. The surgery had to be completed in under ten minutes.
Today we have the luxury of the cardiopulmonary bypass machine, and can attempt more complex repairs. Closure is indicated for all significant ASDs (Qp:Qs >1.5) and should be performed by 4-5 years of age to prevent pulmonary vascular disease. Contraindications to closure include small, hemodynamically insignificant ASDs without cardiomegaly, severe LV failure, and irreversible pulmonary.
Device closure at catheterization has become increasingly popular while surgical closure primarily or with a patch (‘tanned’ or treated pericardium) can be accomplished with low morbidity.