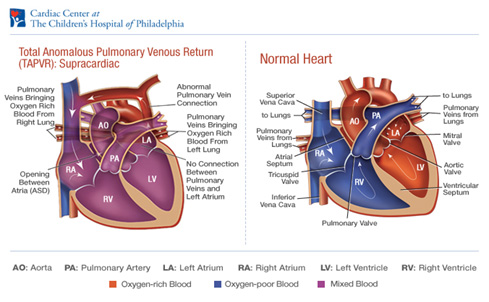
Total Anomalous Pulmonary Venous Return (TAPVR)
In TAPVR the entire pulmonary venous circulation drains to the RA, either directly or by a systemic vein or sinus connecting with the RA via the SVC, IVC, or coronary sinus. An ASD is necessary to deliver oxygenated blood to the left heart. TAPVR is classified as supracardiac, cardiac, or infracardiac. In the most common variant of supracardiac TAPVR, all four pulmonary veins drain into a common, left vertical vein, which then drains into the innominate vein, azygous vein, SVC, or RA. . The classic CXR finding is that of a “snowman” or “figure-of-eight” due to the large vertical vein on the left and SVC on the right In the cardiac subtype, pulmonary venous drainage is into the coronary sinus. In the infracardiac variant, a vertical vein descends below the diaphragm, where it usually connects with the portal vein and then into the IVC.
In cases without obstruction there is a large left-to-right shunt and patients present with heart failure months after birth up to early childhood. There may be a gallop or faint systolic murmur secondary to increased flow across the tricuspid valve, and a prominent fixed S2. Patients with non obstructed TAPVR are repaired electively when diagnosed, usually when symptoms develop around 6 months of age. When there is pulmonary venous obstruction, infants present in extremis within hours to days of birth; they are profoundly cyanotic and in severe congestive heart failure. There is marked pulmonary vasculature and edema on CXR. Diagnosis and mapping of the anomalous connections is possible by echocardiography. Obstructed TAPVR is a surgical emergency. Patients require intubation with 100% oxygen, hyperventilation, and correction of acidosis. ECMO has been used as a temporizing measure. 5-15% of patients develop recurrent pulmonary venous obstruction within the first year post-op.